Purdue University researchers have been successful in focusing at the cell of interest among a background of equally noisy and boisterous biomolecules and other metabolically active cells. Currently, researchers use immunological techniques to create an antibody to a molecule and then visualize the ‘molecule of interest’ by tagging the antibody to a radioisotope or a fluorescent dye; and flow cytometry can sort out different types of cells.
The Purdue University team used gold coated nanoparticles with an iron oxide core that was impregnated in the cell they wished to see. They then subjected the specimen to a periodically changing magnetic field. The superparamagnetic cores (superparamagnetic nanoparticles have no net magnetization, but an external magnetic field can magnetize them) responded by rotating as the magnetic field rotated around them. The rotation could be seen in the ‘near infra-red’ light spectrum, as the incident light bounced off (scattered) the specially designed arms of the gold nanostar as it revolved. The rate (rpm) of this gyromagnetic (gyros means to rotate) twinkling could be externally controlled by varying the rate of the externally applied field. You now could identify the cell by its characteristic ‘twinkling’ (lighthouse type) effect.
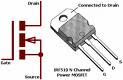
I am tempted to go beyond what’s been achieved so far. Here I go. I guess you are all familiar what happens to the rotating ceiling fan blades when you turn on a fluorescent lamp. Don’t you see a momentary snapshot of the three blades (some have 4)? That’s what where stroboscope comes in. It consists of a Xenon lamp (ordinary fluorescent lamps could do, but incandescent lamps won’t work as the glowing filament takes time to extinguish) flashing at a controllable rate. The electronic circuitry may be had here.
Suppose that the fan is revolving at 1200 RPM and it is not changing. Set your stroboscope to flash at this rate. You’ll ‘see’ that the fan blades are absolutely not moving, which is certainly not true! But be there any mechanical defect in the fan, it will stand out as the centrifugal force widens it (provided that the fault is more or less tangential to the axis of rotation). Here also we are looking at our object of interest, aren’t we?
Now lets look what implication it might have in biological imaging. We now know that
.png) the gamma subunit of mitochondrial F type ATP Synthase ‘actually’ rotates when it is synthesizing ATP (reverse rotation occurs when ATP is hydrolyzed). There are other locomotive units within the cell as well. They comprise of actin and myosin based molecular motors. Could we study them using an externally adjustable stroboscope? The optical (electromagnetic) signals so obtained may then be similarly broken down into simpler trigonometric (sine and cosine) functions by Fourier analysis (Fourier transform) as was done in the ‘twinkling nanostars’ experiment. At least, we expect to get rid of some 'noise' and some good still photos. But if we wanted better resolution and used higher frequency (electromagnetic) for it, some extraneous error will be introduced. It's a trade-off!
the gamma subunit of mitochondrial F type ATP Synthase ‘actually’ rotates when it is synthesizing ATP (reverse rotation occurs when ATP is hydrolyzed). There are other locomotive units within the cell as well. They comprise of actin and myosin based molecular motors. Could we study them using an externally adjustable stroboscope? The optical (electromagnetic) signals so obtained may then be similarly broken down into simpler trigonometric (sine and cosine) functions by Fourier analysis (Fourier transform) as was done in the ‘twinkling nanostars’ experiment. At least, we expect to get rid of some 'noise' and some good still photos. But if we wanted better resolution and used higher frequency (electromagnetic) for it, some extraneous error will be introduced. It's a trade-off!Reference: hyper-links, unless specifically mentioned
Principles of Biochemistry, Lehninger, 4th ed
http://en.wikipedia.org/wiki/ATP_synthase
Wei, Q., Song, H., Leonov, A., Hale, J., Oh, D., Ong, Q., Ritchie, K., & Wei, A. (2009). Gyromagnetic Imaging: Dynamic Optical Contrast Using Gold Nanostars with Magnetic Cores Journal of the American Chemical Society, 131 (28), 9728-9734 DOI: 10.1021/ja901562j